Distance, workforce shortages complicate mental health access in rural Nevada communities
Content notice: This article discusses suicide, suicidal ideation and suicide attempts. If you or a loved one are struggling, it’s OK to share your feelings, and there is free and confidential 24-hour support available in Spanish and English at the 988 suicide and crisis phone line. For mental and behavioral health services in Nevada, click here.
This is the second in our multipart ‘We’ve got to talk’ series, which focuses on youth mental health in Nevada and is produced as part of the USC Annenberg Center for Health Journalism’s 2024 National Fellowship Kristy Hammam Fund for Health Journalism.
You can read the first story here.
The remote ranching community of Wells, at the intersection of Interstate 80 and Highway 93 in the state’s northeastern Elko County, offers examples of the culture of self-reliance, lack of mental health providers and limited privacy that can often hinder discussions of mental health and outreach for help in rural areas.
Reagan Brandt, 16, a cheerleader and Future Farmers of America (FFA) member, said when her parents grew up, they didn’t learn about mental health issues or how to navigate them.
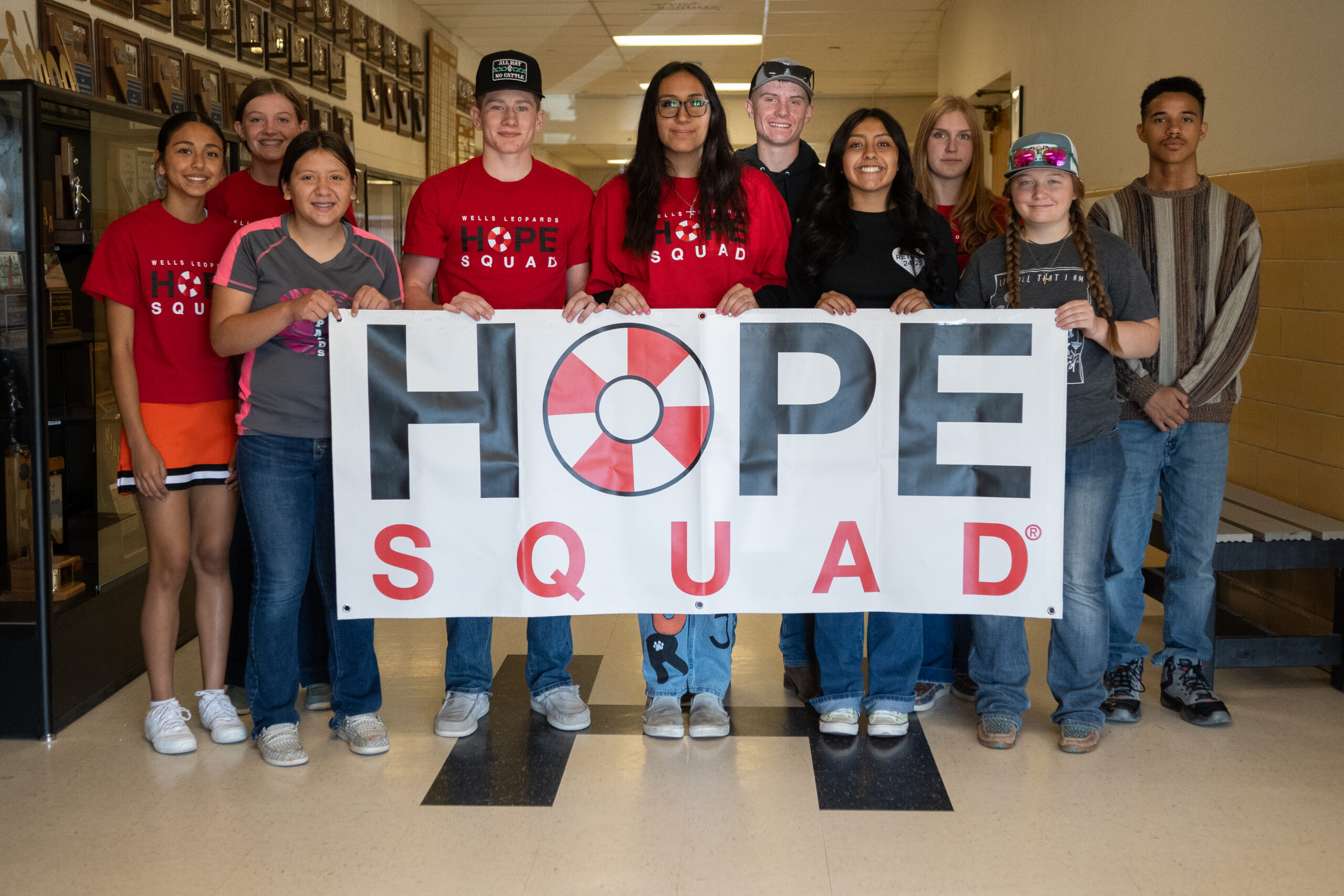
But she and other students at the town’s 110-year-old school are changing that perception through a peer-to-peer support program, Hope Squad, implemented about a year ago.
“As a kid, I just kind of thought, well, maybe I shouldn't be feeling like that,” said Brandt, a member of the Hope Squad. “I came to realize that not everyone’s going to be perfect, and everyone has their own issues.”
As part of the support program, Brandt and other students are trained to spot suicide warning signs, lend a listening ear and communicate with peers struggling with mental health. Based on a set of guidelines taught as part of the program, they refer students facing a mental health crisis to an adult who can establish a safety plan and provide additional resources to the student.
“You have to pay attention to those little things,” said Hope Squad member Aryanna Rodriguez, 15, who plays basketball, volleyball and softball.

Wearing bright red T-shirts with the words “Hope Squad” across the front and a cartoon lifebuoy in place of the “o,” group members are recognizable. Their conversations and awareness extend beyond the schoolyard.
Many speak with the adults in their lives about mental health and work to destigmatize conversations surrounding the topic. When a local grocery store clerk asked one of the members about the shirt and learned about the group, she thanked them for their work.
“We need to stop making [mental health] a separate and such a devised thing,” said Aron Hansen, 15, a Hope Squad and FFA member who plays basketball. “Make it a daily conversation and something that we need to bring up.”
The program is based on research that peer supportive services help students feel less burdened about confiding in a peer and offer a greater sense of belonging. It also builds connectedness, a vital part of suicide prevention and positive mental health outcomes.
Carissa Pearce, the Children’s Advocacy Alliance of Nevada health policy manager, said although peer-to-peer support programs are an important part of meeting mental health needs, there has to be a coordinated network of services and support for youth that includes prevention and early intervention, home and community-based services, crisis services, inpatient treatment and culturally responsive services.
But meeting youth mental health needs is complicated in a state without a unified children’s behavioral and mental health system of care, with geographically isolated communities with limited public transportation and where behavioral and mental health services are heavily reliant upon federal funding.
The challenges with addressing behavioral and mental health needs are further compounded in Nevada by a severe shortage of medical professional services. As of 2023, nearly 86.9 percent of the state’s population lives in a federally designated mental health professional shortage area; there are shortages in every county.

A 2023 UNR report estimates that the state needs more than 1,694 mental health workers in outpatient health and substance abuse centers to meet the national average. In schools, a 2022 UNLV Brookings Mountain West report indicates Nevada has just 26.8 percent of the recommended number of school psychologists and only 2.9 percent of the recommended number of school social workers.
The lack of providers and access issues are seen in Nevada’s ranking as last in the country for overall youth mental health based on the prevalence of mental illness, access to services, insurance coverage and other factors.
“What ends up happening is that people in rural communities who need extra support are having to either drive to urban communities or even try to go somewhere out of state and then just pay out of pocket for receiving services,” Pearce said. “With mental health, that’s something that should be ongoing community-based support.”



Ongoing efforts
In interviews with parents, teachers and staff members in the Elko County School District, many asked about the potential for a youth-focused crisis stabilization center or care that could be closer than their existing options in Salt Lake City, Reno or Las Vegas.
Crisis stabilization centers are being built in Washoe and Clark counties with the support of federal COVID-19 aid, but experts say it’s difficult to establish those options in rural Nevada, where the population is much smaller than in more urban parts of the state.

Steve Simpson, CEO of Northeastern Nevada Regional Hospital in Elko County, said the hospital serves about 40,000 to 45,000 people in the area and is a full-service hospital offering general surgery, orthopedics, OB-GYN options and other practices. He said there’s a pediatrician on staff and opportunities to bring in support or transport patients to hospitals with a higher level of care as needed.
Simpson said the regional hospital is building a 16-bed adult inpatient behavioral health unit, which is expected to open the first week of January.
Patients, he said, can stay in the units long term to receive the care they need. Though the behavioral health wing isn’t open to youth, Simpson said “that’s coming down the pike.”
Establishing such a project presents challenges, he said, including recruiting and retaining qualified professionals — and their spouses — to rural Elko County. These are in addition to delays and challenges presented by the construction and permitting process itself.
“[An inpatient behavioral health unit that focuses on the youth population] is sorely needed,” Simpson said. “What that looks like here yet, I don’t know, but we’re going to have to do something.”
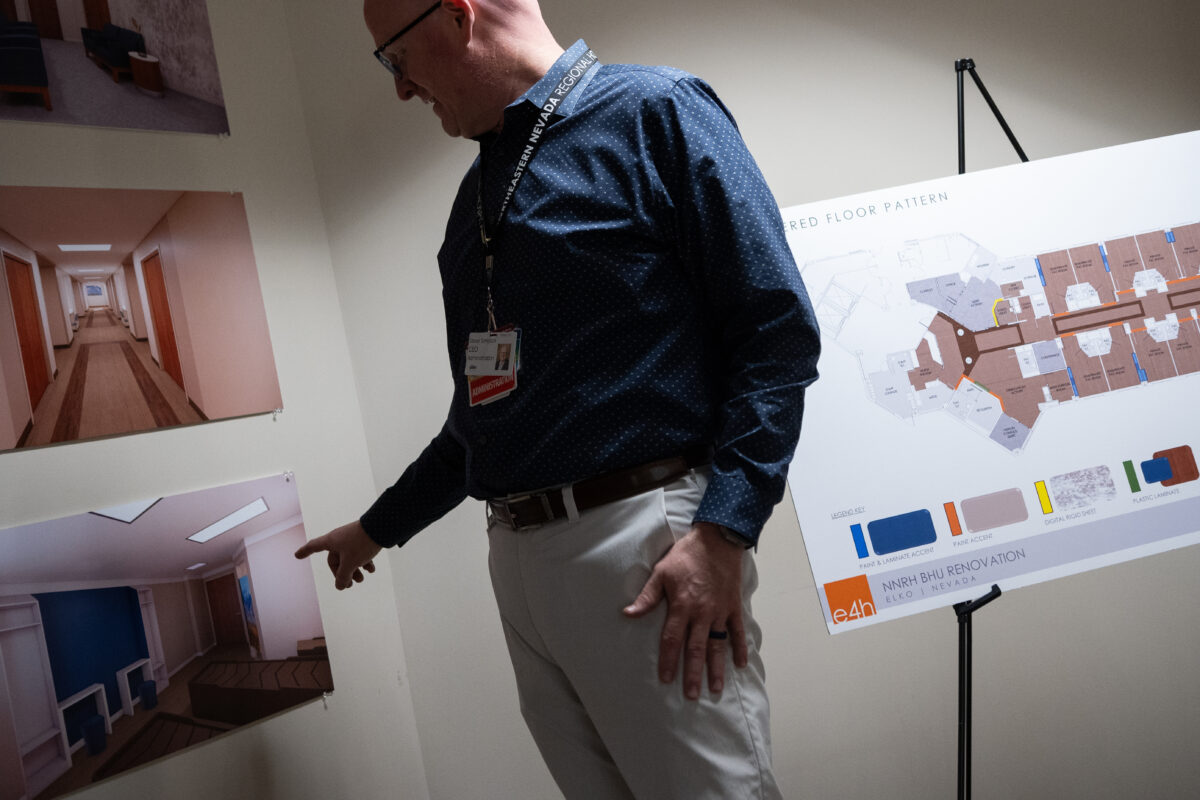

On an average monthly basis, Simpson said the hospital has to transfer about 20-24 patients to a higher level of inpatient mental health care. Many of those patients are repeats. He said the majority of those patients travel to Las Vegas, a more than six-hour trip by car that can be stressful for someone who is already struggling. The new unit is designed to help.
Simpson said that, fortunately, the stigma associated with behavioral mental health issues is dissipating. But in a hospital that is roughly a three-and-a-half-hour car ride from Salt Lake City in the east and about four hours from Reno to the west, it’s important to provide acute resources where travel is challenging.
“I think the willingness to seek help is going to increase,” Simpson said. “My gut tells me that we need to be there at some point, and we want to be a part of that.”

Continued conversations and connecting to resources
Ana Bribiesca, a sergeant for the Elko County Sheriff’s Department and a supervisor for the Elko County School District's school resource officer program, helped the school district implement the Hope Squad initiative. She said she and district officials knew that kids didn’t always want to talk to adults, and this could be a way to help guide conversations and have students help one another.
“We're trying to teach kids to have a voice and help each other out, instead of being ashamed of it like we have when we were growing up,” she said.
A doll of the Disney character Joy from the movie Inside Out sits next to Bribiesca in her car as she checks in with leaders of the groups at different Elko County schools about once a month. The doll reminds her that it’s OK to have emotions.
Brigett Morrison, a social worker who serves as Wells Combined School’s safe school professional and one of the Hope Squad adults, said the school has had the freedom to build its program to meet the needs of its students.

Morrison, along with Ryan Vallejo, who serves as the attendance and registrar and student guidance counselor, and Myles Baldwin, a physical education and health teacher and the school’s athletic director, works with students in Hope Squad to triage responses to crises and ensure that students have access to the resources they need.
Vallejo said if a member of the Hope Squad recognizes a serious situation, such as a student experiencing suicidal ideation, the student has been trained to go through a process of questioning, persuading and referring. Once the Hope Squad member asks hard questions and persuades a student to get help, they refer the student in crisis to one of the three adults.
The staff assess the situation, report any required information and contact the family to determine the next steps. Morrison said they may call in a mobile crisis unit or work with the family to get a student to an emergency room.
Wells is about an hour from Elko, two hours from Twin Falls and two hours from Salt Lake City. Morrison said students needing to be hospitalized usually go to Salt Lake City. Many families don’t have transportation, she said, so there are steps the school takes, such as finding cash assistance or other means of aid.
“We have to really explore our options and see who we can get them in with, because they need immediate assistance that day,” Morrison said. “A lot of time, the parents will choose and try to find out where their insurance goes, but we help them and walk them through the process.”

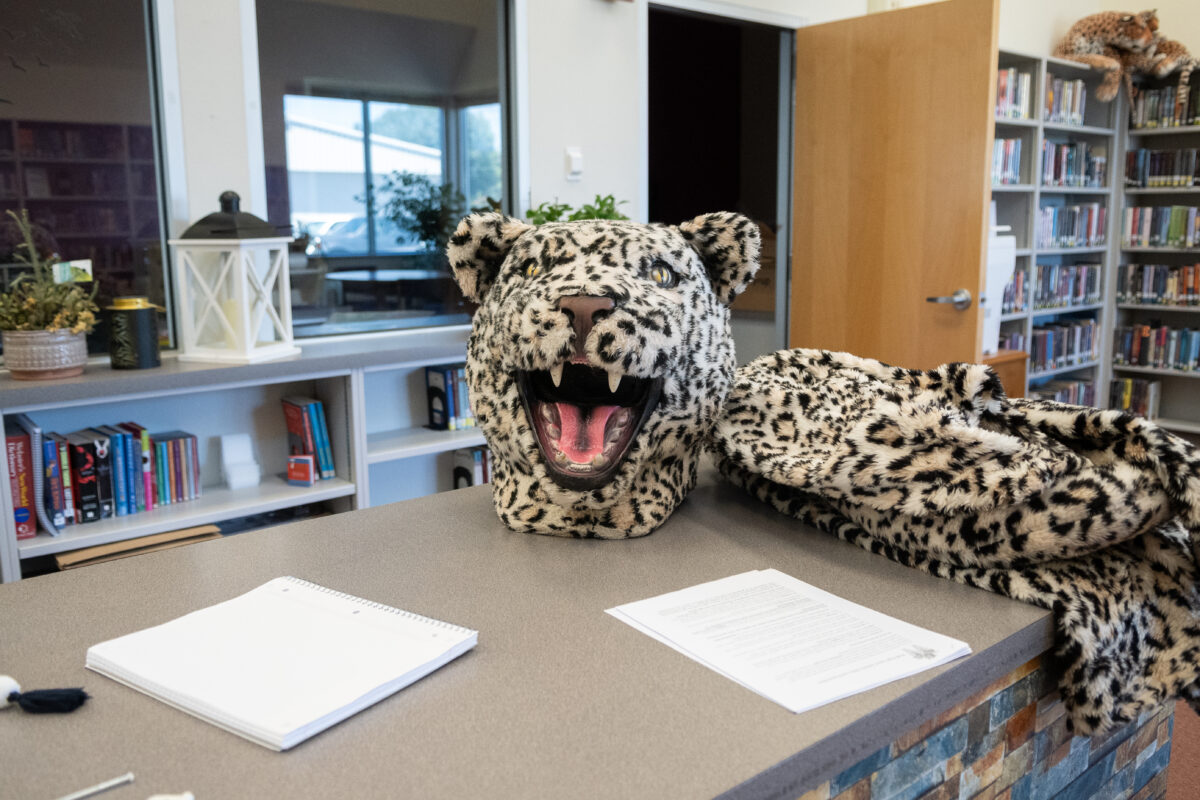
In a school of about 150 students, Baldwin said Hope Squad members take confidentiality requirements seriously.
Baldwin, Vallejo and Morrison said the Hope Squad has increased awareness of mental health needs in the small rural community, shifted respect for mental health, reduced flippant remarks about suicide and helped students develop empathy.
“Within our career choices, [mental health] has always been a part of our jobs,” Vallejo said. “Recognizing now the importance of it, the increased need for it, awareness for it, [the Hope Squad] has definitely opened my eyes.”
